What is Frozen shoulder?
It’s a medical condition characterized by severely reduced range of motion of the shoulder.
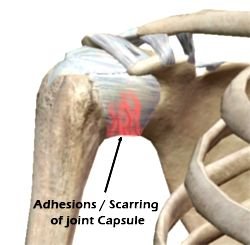
Also known as adhesive capsulitis.
Usually occurs in people over 40 years of age.
If you suffer from diabetes, heart disease, connective tissue disorders or have had a stroke or a severe injury, then you are more at risk of getting frozen shoulder.
What causes Frozen Shoulder Syndrome?
The exact cause is unknown and there are several theories about its cause. Many physicians believe the causes are linked to myo-fascial trigger points associated with the muscles of the shoulder. Slowly the muscles become less flexible and the corresponding shoulder joint gradually becomes locked into place over a period of time.
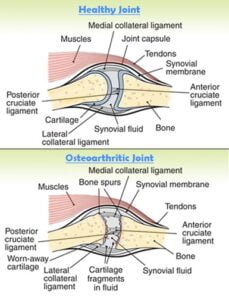
Frozen shoulder may also occur due to inflammation of the joint lining which causes scar tissue to form around the joint. This scar tissue restricts movement in the shoulder causing it to “freeze” and can be very painful.
It’s also believed incomplete healing of a previous shoulder injury can lead to frozen shoulder as the initial injury creates a buildup of scar tissue and inflammation in the shoulder joint.
The main symptoms are:
- Decreased motion of the shoulder
- Stiffness
- Pain
- Night cramps
Frozen Shoulder usually starts with pain. This pain prevents the patient from moving their arm. Lack of movement leads to stiffness and eventually less motion. Over time, you become unable to do movements such as reaching over your head or behind you.

If you have any of the above symptoms you should immediately see an Orthopedic surgeon.
Depending on your condition your doctor can prescribe you the following treatment options:
Conservative treatment options:
- Anti-inflammatory medication
- Physical therapy (physiotherapy)
- Steroid injections
In some cases, it may only take a few weeks to see progress, but in others, it may take as long as 6 – 9 months for complete recovery. Physical therapy is required in some cases and it can be intense, needing to be done every day.
Surgical treatment options:
Surgery is recommended if nonsurgical treatment is not effective.
In cases of moderate to severe frozen shoulder only manipulation under anesthesia may be attempted. The patient is put to sleep using general anaesthesia and the shoulder is manipulated to its full range using controlled force. This procedure takes only 10-15 minutes.
In some severe cases shoulder arthroscopy is done under anesthesia. During this surgery, the scar tissue is released by bringing the shoulder through a full range of motion. Arthroscopic surgery can also be used to cut the tight ligaments and remove the scar tissue from the shoulder. After surgery, the patient may receive pain blocks so they can participate in physical therapy.
Whatever the choice of treatment, physical therapy is very important for full recovery.
Prognosis
Treatment with only physical therapy and non steroidal anti-inflammatory drugs will usually restore motion and function of the shoulder within 6 months. Recovery is faster if treatment is started early.
After surgery restores motion, patients must continue physical therapy for several weeks or months to prevent the frozen shoulder from returning. Treatment may fail if you cannot keep up with physical therapy. Surgery has the potential to speed recovery and improvement in range of motion.
Prevention of frozen shoulder
One of the most common causes of frozen shoulder is the immobility that may result during recovery from a shoulder injury, broken arm or a stroke.
If you have had an injury that makes it difficult to move your shoulder, talk to your doctor about what exercises would be best to maintain the range of motion in your shoulder joint before it reaches the frozen shoulder stage. Start a rehab protocol as early as possible.
If you haven’t had a recent shoulder injury and are still experiencing shoulder pain and stiffness that limits your range of motion for an extended period of time, once again contact your doctor for an evaluation. Early treatment and physical therapy can lead to fewer complications and quicker recovery.


 Dr. Manoj Kumar Khemani has over 15 years experience in treating advanced arthritis. He can monitor your condition, adjust your treatment plan as needed, and provide guidance on the
Dr. Manoj Kumar Khemani has over 15 years experience in treating advanced arthritis. He can monitor your condition, adjust your treatment plan as needed, and provide guidance on the