What is Rheumatoid Arthritis (RA)?
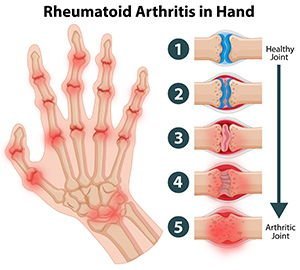
Rheumatoid arthritis one of the commonest type of inflammatory arthritis. In this disease our immune system behaves strangely and starts attacking the tissues of the joints (autoimmune disease). The result is that there is marked swelling and pain in the joints followed by irreversible destruction of the joint.
Women are more affected than men. The disease most often begins between the ages of 30 and 50. However, RA can start at any age.
Clinical presentation of Rheumatoid Arthritis.
Patients of RA have joint pain, stiffness, swelling and decreased movement of the joints. This pain is chronic in nature with episodes of aggravation and remissions. Small joints in the hands and feet are most commonly affected. Rarely RA can affect organs, such as eyes, skin or lungs.
Over a period of the time the pain gets worse and characteristic deformities start appearing in the joints. There is marked stiffness when getting up from bed in the morning.
Other symptoms seen are:
- Marked weakness
- Low grade fever
- Loss of appetite
- Polyarthralgia
- Firm lumps, called rheumatoid nodules, which grow beneath the skin in places such as the elbow and hands
- Anemia
It is commonly seen in middle aged females but can affect people of all ages.
The cause of RA is not known. There is evidence that autoimmune conditions run in families. For instance, certain genes that you are born with may make you more likely to get RA.
Diagnosis of RA.
Diagnosis of RA.
Confirmation of diagnosis is done by one or more investigations:
- Increased RA factor in the blood
- Increased ESR and CRP
- Presence of anti-CCP in blood
- X-Rays
Sometimes more blood tests are done to check if you have other type of arthritis.
Treatment of RA
In the last 30 years there has been significant improvement in the treatment of RA. Current treatments give most patients good or excellent relief of symptoms and let them keep functioning at, or near, normal levels. Treatment is started with a class of medicines called DMARD’s. These medicines help modulate to immune system to minimize inflammatory response. These may be combined with low dose corticosteroids.
Historically gold containing medicines have been used to control RA. However these have been largely abandoned due to potential side effects.
Newer medicines called “Biologic agents” have shown promise in cases where traditional medicines have failed.
In some patients injection of corticosteroids in the joint helps to reduce the pain.
Patients with advanced arthritis of hip, knee, shoulder and elbow are treated with joint replacement surgery.
Is there a permanent cure for RA?
There is no permanent cure for RA. Treatment is aimed at controlling the pain and inflammation, and minimizing joint destruction. Early diagnosis and treatment is key to successful outcome. Once there is permanent damage to the joint, complete pain relief is difficult.
What should I do if I have RA?
- Take medicines regularly
- Do regular exercise
- Drink plenty of water.
- Apply ice packs over the affected area.
- Regular checkup with an orthopaedic surgeon or rheumatologist.
- Swimming helps to keep the joints mobile.